
What is Cannabis?
Cannabis is made from the dried flowering heads and leaves of a plant called Cannabis sativa. Cannabis contains a complex mix of approximately 60 unique ‘cannabinoids’, along with many other chemical compounds. The main active ingredient responsible for the ‘high’ produced by cannabis is delta-9- tetrahydrocannabinol (THC). Other related substances in cannabis include cannabidiol (CBD) and cannabinol (CBN), each of which has different pharmacological effects. CBD is extracted from the leaves which are present in our formulation.
What is medicinal cannabis?
Medicinal cannabis is a term that refers to legal, high quality, and standardized products prepared under controlled pharmaceutical laboratory conditions from crude or raw cannabis. Crude cannabis is a difficult drug for doctors to prescribe because the dose and potency of the drug in each case are not tested or known. Pharmaceutical preparations of cannabis use modified active components of cannabis in medical formulations, which maximize the therapeutic benefit and minimize side effects. Pharmaceutical preparations, such as a tincture, external application oil, gel, tablet, capsule, or spray, mean the dose and strength of the product can be controlled and standardized.


What is the difference between medicinal and recreational cannabis?
Medicinal cannabis is legally produced under strict pharmaceutical conditions. Doctors and pharmacists know exactly what the medicine contains. The ingredients, potency, and quality of illicit recreational cannabis are untested. Contamination with microbes, pesticides, and heavy metals can occur. Doses are usually taken orally or sublingually (under the tongue). By contrast, illicit cannabis is usually smoked. Smoking is a harmful way of using cannabis. People who smoke cannabis frequently have the same breathing problems as those who smoke tobacco. These differences mean recreational cannabis cannot be described as being ‘medicinal cannabis’.
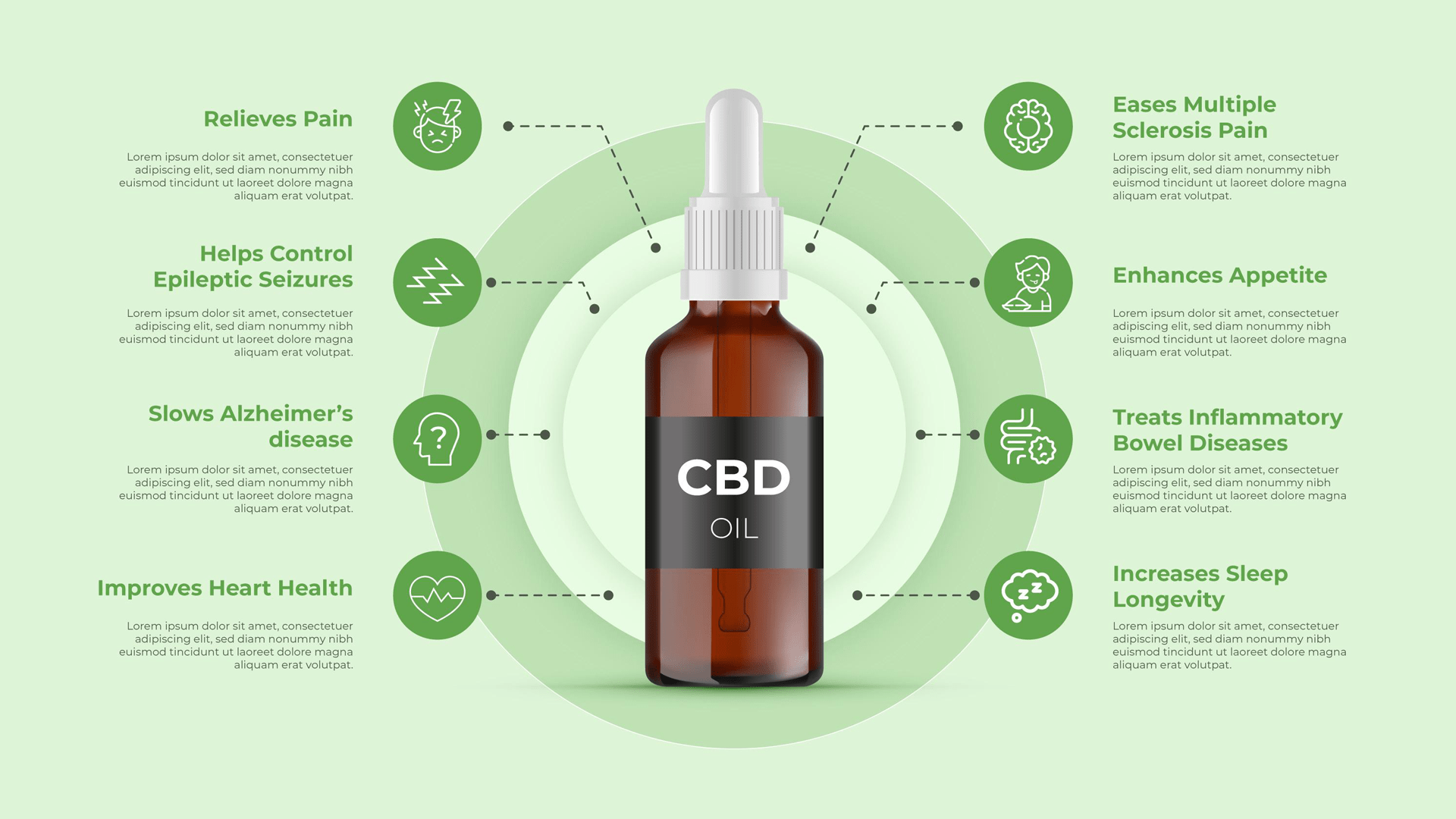
What are the benefits of medicinal cannabis?
Currently, the scientific basis for using medicinal cannabis is limited. There is some evidence it may be useful in the following conditions:
- Treating certain childhood epilepsies
- Treating spasticity and pain in multiple sclerosis
- Treating chronic non-cancer pain
- Relieving chemotherapy-induced nausea and vomiting
What are the side effects of medicinal cannabis?
As with many other medicines, medicinal cannabis can cause unwanted side effects. These side effects include nausea and vomiting, changes in appetite, diarrhea, drowsiness, dizziness, loss of balance, and difficulty with concentration.
Can I drive if I am using cannabis?
Any product that contains cannabis can impair attention and concentration, which affects a person’s fitness to drive and operate machinery. Studies have shown a significant proportion of drivers involved in road crashes test positive for cannabis. It is recommended people using medicinal cannabis as oral intake do not drive. Patients are advised to discuss this with their doctor.


What is medical Cannabis used for?
Researchers are studying whether medical Cannabis can help treat a number of conditions including:
- Alzheimer’s disease
- Appetite loss
- Cancer
- Crohn’s disease
- Diseases affecting the immune system like HIV/AIDS or Multiple Sclerosis (MS)
- Eating disorders such as anorexia
- Epilepsy
- Glaucoma
- Mental health conditions like schizophrenia and post-traumatic stress disorder (PTSD)
- Multiple sclerosis
- Muscle spasms
- Nausea
- Pain
- Seizures
- Wasting syndrome (cachexia)
Mechanism of Action
Cannabinoids function by stimulating two receptors, cannabinoid receptor type 1 (CB1) and type 2 (CB2), within the endocannabinoid system. This system is a complex network of organs throughout the body, expressing the cannabinoid receptors and playing a homeostatic role. Functions of the endocannabinoid system include pain, memory, movement, appetite, metabolism, lacrimation /salivation, immunity, and even cardiopulmonary function. It bears mentioning that the vast majority of end-effects from cannabinoids, including psychotropics, are from activation of CB1, with CB2 serving more important roles in immune and inflammatory functions. Endogenously, endocannabinoids serve as neuro-regulatory modulators responsible for retrograde neurotransmission.

Here, a post-synaptic neuron releases endocannabinoids that bind to predominantly CB1 receptors on the presynaptic neuron. This binding results in inhibited presynaptic calcium channel activation and subsequent presynaptic neurotransmitter release. If the presynaptic neurotransmitters are predominantly inhibitory such as GABA, the net effect is excitatory and vice versa. Binding to the different parts of the central nervous system mediates different psychotropic properties of cannabinoids, particularly THC. These areas and end-effects include:
- Hippocampus: impairment of short-term memory
- Neocortex: impairment of judgment and sensation
- Basal ganglia: altered reaction time and movement
- Hypothalamus: increased appetite
- Nucleus accumbens: euphoria
- Amygdala: panic and paranoia
- Cerebellum: ataxia
- Brainstem: anti-emesis
- Spinal cord: analgesia Other end-effects of CB1 activation peripherally include dry mouth, conjunctivitis, tachycardia, hypotension, and bradypnea.

Adverse Effects
Adverse effects of cannabinoids exist on a spectrum, ranging from mild to lethal, and vary on the mode associated risks of administration. The most frequently encountered side effects of cannabinoids are generally those from recreational sources. Over the short-term, mild effects include euphoria, anxiolysis, tachycardia, visuotemporal distortion, sensory amplification, tachycardia, postural hypotension, conjunctivitis, hunger, and dry throat, mouth, and eyes. More severe symptoms include panic attacks, myoclonus, psychosis, hyperemesis, inhalation burns, acute respiratory distress syndrome (ARDS), and bronchospasm-any one of which may result in hospitalization or the necessity of emergency medical services. Over the long term, heavy cannabinoid abuse has correlated in numerous adverse health conditions, including:
- Addiction, altered brain development, and cognitive impairment in adolescents
- Chronic bronchitis, ARDS, lung cancer
- Increased risk for myocardial infarction, stroke, and thromboembolic events
- Exacerbation of mood disorders (anxiety, depression) and psychotic disorders (schizophrenia)
- Exacerbation of neurodegenerative diseases (multiple sclerosis, Alzheimer’s disease, Parkinson’s disease) In addition to the above, other adverse effects of cannabinoids include hypersensitivity reactions to active cannabinoids in specific formulations or constituent components (e.g., capsules or inactive additives) or disulfiram reaction (nausea, vomiting, abdominal cramping, and headache) with concurrent disulfiram or metronidazole use.
Contraindications
Contraindications to cannabinoids are few but include hypersensitivity to specific medications, cannabinoids generally, constituent components of specific formulations (e.g., sesame seed oil in capsules or other inactive ingredients), and recent administration of products containing disulfiram or metronidazole within two weeks. Some have also posited that concurrent anxiety or mood disorders or personal/family history of psychotic disorders such as schizophrenia may also be a contraindication.


Monitoring
Cannabinoids are generally not monitored regularly except for some patients who require routine drug screening or present with suspicion of drug overdose or abuse. The most common diagnostic test for cannabinoid detection is the urine drug screen (UDS), which detects THC and CBD metabolites. Otherwise, owing to differences in metabolism, mode of administration detection, and frequency of use may cause detection times to vary significantly between patients. Besides UDS, monitoring is otherwise based mainly on symptoms of intoxication and overdose.
Toxicity
In the event of cannabinoid drug toxicity, as described above, treatment and management are largely supportive and focused on symptom relief. Psychosis and agitation should have treatment with benzodiazepines and antipsychotics, preferably of the second-generation or atypical class, due to their lower risk of extrapyramidal effects. An electrocardiogram can rule out myocardial ischemia or dysrhythmias, and if present, the clinician should start empiric therapy with rate-controlling agents. Hyperemesis should receive appropriate medication with antiemetics provided that the risk of dysrhythmias is sufficiently low. Clinicians need to address seizure activity with benzodiazepines and/or anticonvulsant agents as tolerated. Finally, signs of pulmonary compromise should necessitate supportive measures such as oxygen via nasal cannula, positive airway pressure ventilation, and endotracheal intubation if severe enough.


PHARMACOLOGY
Endocannabinoids (eCBs) and their receptors are found throughout the human body: nervous system, internal organs, connective tissues, glands, and immune cells. The eCB system has a homeostatic role, having been characterized as “eat, sleep, relax, forget, and protect.”26 It is known that eCBs have a role in the pathology of many disorders while also serving a protective function in certain medical conditions.27 It has been proposed that migraine, fibromyalgia, irritable bowel syndrome, and related conditions represent clinical eCB deficiency syndromes (CEDS). Deficiencies in eCB signaling could be also involved in the pathogenesis of depression. In human studies, eCB system deficiencies have been implicated in schizophrenia, multiple sclerosis (MS), Huntington’s disease, Parkinson’s disease, anorexia, chronic motion sickness, and failure to thrive in infants.28
The eCB system represents a microcosm of psycho-neuroimmunology or “mind–body” medicine. The eCB system consists of receptors, endogenous ligands, and ligand metabolic enzymes. A variety of physiological processes occur when cannabinoid receptors are stimulated. Cannabinoid receptor type 1 (CB ) is the most abundant G-protein–coupled receptor. It is expressed in the central nervous system, 1 with particularly dense expression in (ranked in order): the substantia nigra, globus pallidus, hippocampus, cerebral cortex, putamen, caudate, cerebellum, and amygdala. CB is also expressed in 1 non-neuronal cells, such as adipocytes and hepatocytes, connective and musculoskeletal tissues, and the gonads. CB is principally associated with cells governing immune function, although it may also be 2 expressed in the central nervous system. The most well-known eCB ligands are N-arachidonyl-ethanolamide (anandamide or AEA) and sn-2-arachidonoyl-glycerol (2-AG). AEA and 2-AG are released upon demand from cell membrane phospholipid precursors. This “classic” eCB system has expanded with the discovery of secondary receptors, ligands, and ligand metabolic enzymes. For example, AEA, 2-AG, N-arachidonoyl glycine 9 (NAGly), and the phytocannabinoids Δ -THC and CBD may also serve, to different extents, as ligands at GPR55, GPR18, GPR119, and several transient receptor potential ion channels (e.g., TRPV1, TRPV2, TRPA1, TRPM8) that have actions similar to capsaicin.28 The effects of AEA and 2-AG can be enhanced by “entourage compounds” that inhibit their hydrolysis via substrate competition, and thereby prolong their action through synergy and augmentation. Entourage compounds include N-palmitylethanolamide (PEA), N-oleoylethanolamide (SEA), and cis-9-octadecenoamide (OEA or oleamide) and may represent a novel route for molecular regulation of endogenous cannabinoid activity.29 Additional noncannabinoid targets are also linked to cannabis. G-protein-coupled receptors provide noncompetitive inhibition at mu and delta opioid receptors as well as norepinephrine, dopamine, and serotonin. Ligand-gated ion channels create allosteric antagonism at serotonin and nicotinic receptors, and enhance activation of glycine receptors. Inhibition of calcium, potassium, and sodium channels by noncompetitive antagonism occurs at nonspecific ion channels and activation of PPAR and PPAR at the peroxisome proliferator-activated receptors is influenced by AEA.30 THC is known to be the major psychoactive component of cannabis mediated by activation of the CB 1 receptors in the central nervous system; however, this very mechanism limits its use due to untoward adverse effects. It is now accepted that other phytocannabinoids with weak or no psychoactivity have promise as therapeutic agents in humans. The cannabinoid that has sparked the most interest as a nonpsychoactive component is CBD.31 Unlike THC, CBD elicits its pharmacological effects without exerting any significant intrinsic activity on CB and CB receptors. Several activities give CBD a high 1 2 potential for therapeutic use, including antiepileptic, anxiolytic, antipsychotic, anti-inflammatory, and neuroprotective effects. CBD in combination with THC has received regulatory approvals in several European countries and is under study in registered trials with the FDA. And, some states have passed legislation to allow for the use of majority CBD preparations of cannabis for certain pathological conditions, despite lack of standardization of CBD content and optimal route of administration for effect.32
Specific applications of CBD have recently emerged in pain (chronic and neuropathic), diabetes, cancer, and neurodegenerative diseases, such as Huntington’s disease. Animal studies indicate that a high dose of CBD inhibits the effects of lower doses of THC. Moreover, clinical studies suggest that oral or oromucosal CBD may prolong and/or intensify the effects of THC. Finally, preliminary clinical trials suggest that high-dose oral CBD (150–600 mg per day) may exert a therapeutic effect for epilepsy, insomnia, and social anxiety disorder. Nonetheless, such doses of CBD have also been shown to cause sedation.
PHARMACOKINETIC AND ADMINISTRATION
The three most common methods of administration are inhalation via smoking, inhalation via vaporization, and ingestion of edible products. The method of administration can impact the onset, intensity, and duration of psychoactive effects; effects on organ systems; and the addictive potential and negative consequences associated with use. Cannabinoid pharmacokinetic research has been challenging; low analyte concentrations, rapid and extensive metabolism, and physicochemical characteristics hinder the separation of compounds of interest from biological matrices and from each other. The net effect is lower drug recovery due to the adsorption of compounds of interest to multiple surfaces.

The primary psychoactive constituent of 9 Cannabis—Δ -THC—is rapidly transferred from the lungs to blood during smoking. In a randomized controlled trial conducted by Huestis and colleagues, THC was detected in plasma immediately after the first inhalation of Cannabis smoke, attesting to the efficient absorption of THC from the lungs. THC levels rose rapidly and peaked prior to the end of smoking. Although smoking is the most common cannabis administration route, the use of vaporization is increasing rapidly. Vaporization provides effects similar to smoking while reducing exposure to the byproducts of combustion and possible carcinogens and decreasing adverse respiratory syndromes. THC is highly lipophilic, distributing rapidly to highly perfused 9 tissues and later to fat. A trial of 11 healthy subjects administered Δ -THC intravenously, by smoking, and by mouth demonstrated that plasma profiles of THC after smoking and intravenous injection were similar, whereas plasma levels after oral doses were low and irregular, indicating slow and erratic absorption. The time courses of plasma concentrations and clinical “high” were of the same order for intravenous injection and smoking, with prompt onset and steady decline over a four-hour period. After oral THC, the onset of clinical effects was slower and lasted longer, but effects occurred at much lower plasma concentrations than they did after the other two methods of administration. Cannabinoids are usually inhaled or taken orally; the rectal route, sublingual administration, transdermal delivery, eye drops, and aerosols have been used in only a few studies and are of little relevance in practice today. The pharmacokinetics of THC vary as a function of its route of administration. Inhalation of THC causes a maximum plasma concentration within minutes and psychotropic effects within seconds to a few minutes. These effects reach their maximum after 15 to 30 minutes and taper off within two to three hours. Following oral ingestion, psychotropic effects manifest within 30 to 90 minutes, reach their maximum effect after two to three hours, and last for about four to 12 hours, depending on the dose. Within the shifting legal landscape of medical cannabis, different methods of cannabis administration have important public health implications. A survey using data from Qualtrics and Facebook showed that individuals in states with medical cannabis laws had a significantly higher likelihood of ever having used the substance with a history of vaporizing Cannabis (odds ratio [OR], 2.04; 99% confidence interval [CI], 1.62–2.58) and a history of oral administration of edible Cannabis (OR, 1.78; 99% CI, 1.39–2.26) than those in states without such laws. Longer duration of medical cannabis status and higher dispensary density were also significantly associated with use of vaporized and edible forms of Cannabis. Medical cannabis laws are related to state-level patterns of utilization of alternative methods of cannabis administration.

DRUG INTERACTIONS
Metabolic and pharmacodynamic interactions may exist between medical cannabis and other pharmaceuticals. Quantification of the in vitro metabolism of exogenous cannabinoids, including THC, CBD, and cannabinol (CBN), indicates hepatic cytochrome 450 (CYP450) isoenzymes 2C9 and 3A4 play a significant role in the primary metabolism of THC and CBN, whereas 2C19 and 3A4 and may be responsible for metabolism of CBD.40 Limited clinical trials quantifying the effect of the exogenous cannabinoids on the metabolism of other medications exist. Concomitant administration of ketoconazole with oromucosal cannabis extract containing THC and CBD resulted in an increase in the maximum serum concentration and area under the curve for both THC and CBD by 1.2-fold to 1.8-fold and twofold, respectively; coadministration of rifampin is associated with a reduction in THC and CBD levels.
MEDICINAL USES
Cannabis and cannabinoid agents are widely used to alleviate symptoms or treat disease, but their efficacy for specific indications is not well established. For chronic pain, the analgesic effect remains unclear. A systematic review of randomized controlled trials was conducted examining cannabinoids in the treatment of chronic noncancer pain, including smoked cannabis, oromucosal extracts of cannabis-based medicine, nabilone, dronabinol, and a novel THC analog. Pain conditions included neuropathic pain, fibromyalgia, rheumatoid arthritis, and mixed chronic pain. Fifteen of the 18 included trials demonstrated a significant analgesic effect of cannabinoids compared with placebo.

Cannabinoid use was generally well tolerated; adverse effects most commonly reported were mild to moderate in severity. Overall, evidence suggests that cannabinoids are safe and moderately effective in neuropathic pain with preliminary evidence of efficacy in fibromyalgia and rheumatoid arthritis. While there is not enough evidence to suggest routine use of medicinal cannabis for alleviating chemotherapy-related nausea and vomiting by national or international cancer societies, therapeutic agents based on THC (e.g., dronabinol) have been approved for use as an antiemetic in the United States for a number of years. Only recently has the efficacy and safety of cannabis-based medicines in managing nausea and vomiting due to chemotherapy been evaluated. In a review of 23 randomized, controlled trials, patients who received cannabis-based products experienced less nausea and vomiting than subjects who received placebo.56
The proportion of people experiencing nausea and vomiting who received cannabis-based products was similar to those receiving conventional antiemetics. Subjects using cannabis-based products experienced side effects such as “feeling high,” dizziness, sedation, and dysphoria and dropped out of the studies at a higher rate due to adverse effects compared with participants receiving either placebo or conventional antiemetics. In crossover trials in which patients received cannabis-based products and conventional antiemetics, patients preferred the cannabis-based medicines. Cannabis-based medications may be useful for treating chemotherapy-induced nausea and vomiting that responds poorly to conventional antiemetics. However, the trials produced low to moderate-quality evidence and reflected chemotherapy agents and antiemetics that were available in the 1980s and 1990s. In older patients, medical cannabinoids have shown no efficacy on dyskinesia, breathlessness, and chemotherapy-induced nausea and vomiting. Some evidence has shown that THC might be useful in the treatment of anorexia and behavioral symptoms in patients with dementia. The most common adverse events reported during cannabinoid treatment in older adults were sedation-like symptoms.
IS IT SAFE FOR A BREASTFEEDING PERSON TO USE CANNABIS?
Breastfeeding persons are encouraged to avoid using Cannabis. The health effects of a breastfeeding person’s use of Cannabis on her infant are not yet fully known, and the available data are limited and conflicting. However, we know that chemicals from Cannabis can be passed to a baby through breast milk. In addition, tetrahydrocannabinol (THC) is stored in body fat and is slowly released over time, meaning that a baby could still be exposed even after a breastfeeding person stops using Cannabis.

